Table of Contents
About This Issue
Epistaxis, or bleeding from the nose, is a common presenting condition in the urgent care. First-line treatment begins with compression over the distal nasal bones and progresses to topical decongestants, cautery, and nasal packing. Recognizing posterior epistaxis and certain circumstances such as patients with significant head or facial trauma, certain disorders or conditions, or uncontrolled bleeding is critical for urgent care clinicians to obtain effective clinical outcomes. In this issue, you will learn:
How the etiology and physical examination guides management
How to differentiate between anterior and posterior epistaxis and how they commonly present
Which treatments are efficient in stopping bleeding quickly
What conservative measures, progressing to more invasive methods, limit bleeding, as well as how to approach treatment in special populations
Which conditions warrant emergency department evaluation or referral to an otolaryngologist
CODING & CHARTING: Coding a patient encounter for epistaxis is guided by the complexity of the presentation and treatment. Learn more in our monthly coding column.
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Etiology and Pathophysiology
- Differential Diagnosis
- Urgent Care Evaluation
- Diagnostic Studies
- Treatment
- Anterior Epistaxis
- Posterior Epistaxis
- Special Populations
- Patients With Hypertension
- Pregnant Patients
- Patients With Certain Disorders
- Patients Taking Anticoagulants
- Nasal Injuries
- Foreign Bodies
- Controversies/Cutting Edge
- Tranexamic Acid
- Prophylactic Antibiotics
- Disposition
- Summary
- Risk Management Pitfalls to Avoid in the Urgent Care Management of Epistaxis
- Time- and Cost-Effective Strategies
- Critical Appraisal of the Literature
- 5 Things That Will Change Your Practice
- KidBits: Epistaxis in Children
- Etiology, Pathophysiology, and Differential Diagnosis
- Urgent Care Evaluation
- Initial Presentation
- History
- Physical Examination
- Diagnostic Studies
- Treatment
- Summary
- Case Conclusions
- Coding & Charting: What You Need to Know
- Problems Addressed
- Complexity of Data
- Risk of Patient Management
- Coding Challenge: Epistaxis in Urgent Care
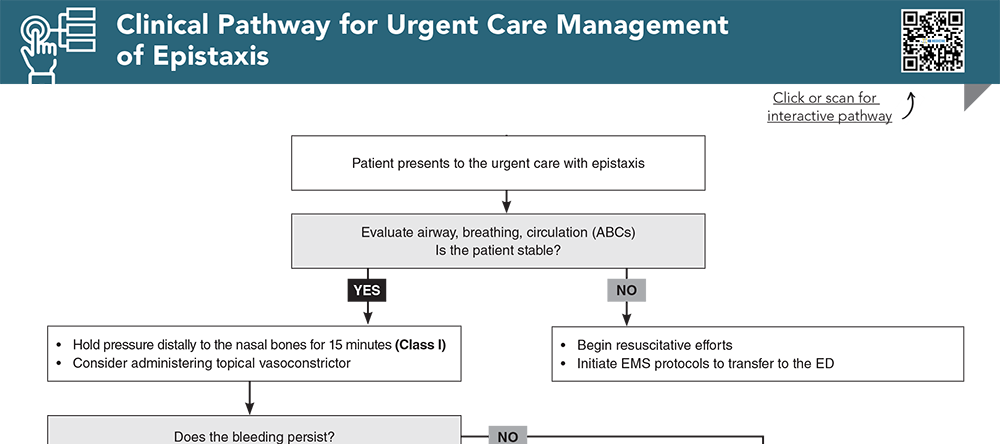
- Clinical Pathway for Urgent Care Management of Epistaxis
- References
Abstract
Epistaxis, or bleeding from the nose, is a common presentation in the urgent care setting, and it can be distressing for patients. Although most cases resolve without complicated intervention, patients may seek medical care if bleeding is severe, refractory, or recurrent. Unusual conditions that present with epistaxis can be serious; therefore, the urgent care clinician should be familiar with the wide differential diagnosis to aid in distinguishing between the benign causes of epistaxis and those that require referral to the emergency department. This review discusses the various etiologies of epistaxis, along with evaluation and management recommendations for patients with epistaxis.
Case Presentations
- The patient states the bleeding started spontaneously earlier in the day as he was watching television. He denies any history of recurrent nosebleeds.
- He states he has not put anything in his nose such as nasal sprays, saline rinses, or his fingers. He denies any recent trauma or injury.
- It is currently summer.
- He has not missed any doses of his medications and has not been on any new medications recently. He denies any new changes to his diet.
- He attempted to hold pressure on his nose at home, which did not abate the bleeding.
- He denies light headedness or dizziness.
- You wonder if this patient should be referred to the ED…
- The patient’s mother states the patient has had nosebleeds several times lately. The bleeding today was concerning to the patient’s mother because this was the sixth nosebleed the patient has had in the past 2 weeks.
- The patient is typically able to resolve the bleeding on her own by holding pressure.
- The patient does not have a history of recurrent nosebleeds or any recent trauma.
- Should this patient be seen by an otolaryngologist?
- The patient’s mother states the patient sometimes has nosebleeds that typically self-resolve.
- The mother attributes the previous nosebleeds to dry air in the home, and she has been running a humidifier.
- The patient’s mother states today the patient accidentally rolled off the couch and then started to bleed from his nose. He did not have any loss of consciousness and cried immediately.
- The patient appears irritable.
- What additional history and physical examination findings should you be looking for?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Managing Patients Presenting with Acute Diarrhea in Urgent Care
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
1. * Pallin DJ, Chng YM, McKay MP, et al. Epidemiology of epistaxis in US emergency departments, 1992 to 2001. Ann Emerg Med. 2005;46(1):77-81. (Cross-sectional study; 4,503,000 emergency department visits) DOI: 10.1016/j.annemergmed.2004.12.014
2. * Womack JP, Kropa J, Jimenez Stabile M. Epistaxis: outpatient management. Am Fam Physician. 2018;98(4):240-245. (Review) PMID: 30215971
3. * Krulewitz NA, Fix ML. Epistaxis. Emerg Med Clin North Am. 2019;37(1):29-39. (Review) DOI: 10.1016/j.emc.2018.09.005
12. * Smith J, Hanson J, Chowdhury R, et al. Community-based management of epistaxis: who bloody knows? Can Pharm J (Ott). 2019;152(3):164-176. (Review) DOI: 10.1177/1715163519840380
Subscribe to get the full list of 27 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: epistaxis, nosebleeds, hereditary hemorrhagic telangiectasias, bleeding disorders, nasal packing, nasal cautery, nasal trauma, anterior epistaxis, posterior epistaxis, facial trauma