Table of Contents
About This Issue
Ear complaints are a common reason for pediatric patients to present to the emergency department. The clinical presentation for ear complaints can often overlap with other common pediatric diseases and, therefore, it is important to always consider ear concerns as part of a differential diagnosis. A systematic approach will improve the accuracy of diagnoses and the appropriateness of management. This issue provides an evidence-based approach to the diagnosis, workup, and management of common pediatric ear complaints including acute otitis media, acute otitis externa, acute mastoiditis, and foreign bodies in the ear canal. In this issue, you will learn:
Common causes of ear infections
Conditions in the differential diagnosis of pediatric ear complaints
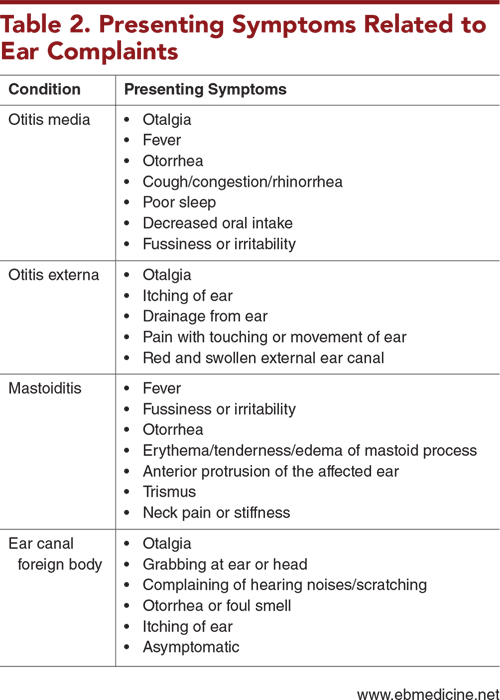
Presenting symptoms related to ear complaints
Important considerations when obtaining the history
Approaches that can help ensure an effective examination
Caregiver holds that can facilitate an ear examination
When laboratory and imaging studies are indicated
Management recommendations for acute otitis media, acute otitis externa, mastoiditis, and ear canal foreign bodies
Which patients can be safely discharged home and which patients should be admitted
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Etiology and Pathophysiology
- Anatomy of the Ear
- Acute Otitis Media
- Acute Otitis Externa
- Mastoiditis
- Ear Canal Foreign Bodies
- Differential Diagnosis
- Acute Otitis Media
- Acute Otitis Externa
- Mastoiditis
- Ear Canal Foreign Body
- Cholesteatomas
- Prehospital Care
- Emergency Department Evaluation
- History
- Physical Examination
- Helpful Holds During the Ear Examination
- Ear Canal and Tympanic Membrane Examination
- Pneumatic Otoscopy
- Periauricular Skin and Tissue Examination
- Additional Considerations
- Diagnostic Studies
- Laboratory Studies
- Imaging Studies
- Treatment
- Acute Otitis Media
- Management of Patients With Myringotomy Tubes
- Management of Patients With Ruptured Tympanic Membrane
- Acute Otitis Externa
- Mastoiditis
- Ear Canal Foreign Bodies
- Special Populations
- Controversies and Cutting Edge
- Disposition
- Acute Otitis Media and Acute Otitis Externa
- Mastoiditis
- Ear Canal Foreign Bodies
- Risk Management Pitfalls for Children With Ear Complaints Presenting to the Emergency Department
- 5 Things That Will Change Your Practice
- Summary
- Time- and Cost-Effective Strategies
- Case Conclusions
- Clinical Pathways
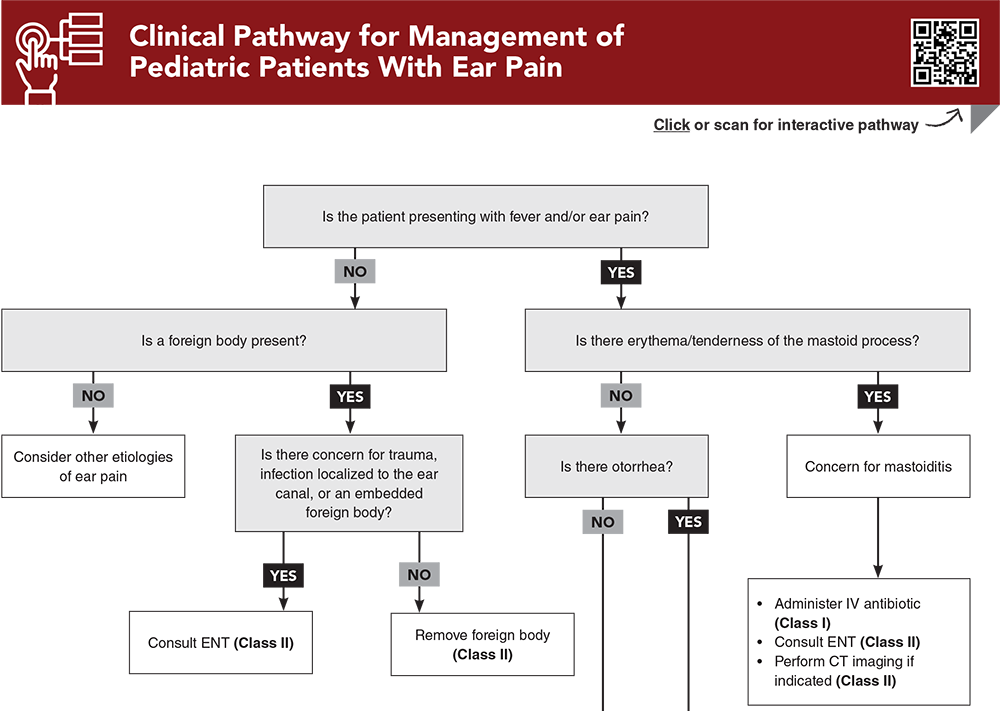
- Clinical Pathway for Management of Pediatric Patients With Ear Pain
- Clinical Pathway for Management of Pediatric Patients Presenting With Ear Canal Foreign Bodies
- Videos
- Tables and Figures
- References
Abstract
The clinical presentation for ear complaints can often overlap with other common pediatric conditions. As such, the differential diagnosis for ear complaints is broad, warranting a thorough history and targeted physical examination. Optimizing the approach for a definitive ear examination is essential when evaluating a pediatric patient with an ear concern. A systematic approach will improve the accuracy of diagnoses and the appropriateness of management. This issue provides an evidence-based approach to the diagnosis, workup, and management of common ear complaints in pediatric patients.
Case Presentations
- Her parents report that she has been crying more than normal over the past 2 days. They tell you she has decreased oral intake and that she is drooling more than normal. Her maximum temperature at home was 39.1°C. Her parents also report she has been sick recently with cough and congestion, though those symptoms have since improved.
- On examination, you note the patient is overall well-appearing but hesitant to examination, and she cries as you approach.
- What clinical findings would point you toward an ear-related underlying diagnosis?
- The patient has had a fever for the past 7 days, despite currently being treated with amoxicillin for an ear infection. During this time, the patient has been more fussy than normal, with decreased oral intake. His parents deny any rashes or skin changes but do report that his left ear appears to be sticking out more than normal. They tell you he has not had any cough, congestion, vomiting, or diarrhea.
- The boy is febrile and tachycardic, but his vital signs are otherwise stable. You find the patient to appear uncomfortable on examination and difficult to console.
- How should you approach the workup?
- The family reports that the boy woke up this morning and started complaining of hearing noises that the family cannot hear. He has no history of similar concerns, and the family denies access to medications in their house. The parents report that their son has not been sick recently.
- On evaluation, you note the patient is holding his head and seems irritated. He is afebrile with no signs of respiratory distress. There is no report to indicate ingestion or intoxication.
- How should you approach the management of this patient?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Management of Pediatric Patients With Ear Pain
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
4. * Lieberthal AS, Carroll AE, Chonmaitree T, et al. The diagnosis and management of acute otitis media. Pediatrics. 2013;131(3):e964-e999. (Clinical practice guidelines) DOI: 10.1542/peds.2012-3488
18. * Psarommatis IM, Voudouris C, Douros K, et al. Algorithmic management of pediatric acute mastoiditis. Int J Pediatr Otorhinolaryngol. 2012;76(6):791-796. (Retrospective; 167 patients) DOI: 10.1016/j.ijporl.2012.02.042
22. * Acevedo JL, Lander L, Shah UK, et al. Existence of important variations in the United States in the treatment of pediatric mastoiditis. Arch Otolaryngol Head Neck Surg. 2009;135(1):28-32. (Retrospective; 1049 patients) DOI: 10.1001/archoto.2008.510
28. * Prasad N, Harley E. The aural foreign body space: a review of pediatric ear foreign bodies and a management paradigm. Int J Pediatr Otorhinolaryngol. 2020;132:109871. (Observational; 155 patients) DOI: 10.1016/j.ijporl.2020.109871
30. * American Academy of Family Physicians, American Academy of Otolaryngology-Head and Neck Surgery, American Academy of Pediatrics Subcommittee on Otitis Media With Effusion. Otitis media with effusion. Pediatrics. 2004;113(5):1412-1429. (Clinical practice guidelines) DOI: 10.1542/peds.113.5.1412
31. * Smith ME, Hardman JC, Mehta N, et al. Acute otitis externa: consensus definition, diagnostic criteria and core outcome set development. PLoS One. 2021;16(5):e0251395. (Consensus guidelines) DOI: 10.1371/journal.pone.0251395
40. * Mui S, Rasgon BM, Hilsinger RL Jr, et al. Tympanostomy tubes for otitis media: quality-of-life improvement for children and parents. Ear Nose Throat J. 2005;84(7):418, 420-412, 424. (Retrospective; 379 patients) DOI: 10.1177/014556130508400712
Subscribe to get the full list of 57 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: acute otitis media, AOM, acute otitis externa, AOE, mastoiditis, ear foreign body, ear canal foreign body, myringotomy tubes, tympanostomy tubes, tympanic membrane, perforated tympanic membrane, ear infections, ear pain, pediatric ear, ear canal, otorrhea, ear effusion, caregiver holds, chest-to-chest hold, side-to-chest hold, pneumatic otoscopy