Table of Contents
About This Issue
Identifying the source of otalgia in emergency department patients is key in differentiating serious and dangerous conditions from common, benign causes, and will allow emergency clinicians to offer safe and effective treatment options. In this issue, you will learn:
How to tell acute otitis media from otitis media with effusion, and the best treatments for each.
Which acute otitis externa (“swimmer’s ear") treatments to prescribe, and which ototoxic medications to avoid.
What to look for in the tympanic membrane, and how its appearance can be used to initiate appropriate treatment.
How to determine whether a “wait-and-see” antibiotic prescription is the best management strategy.
The essential elements of the otoscopic assessment.
The comorbid conditions that are red flags for necrotizing (“malignant”) otitis externa, and when IV antibiotic therapies should be initiated.
The telltale sign of perichondritis, and when admission for IV therapy and/or incision and drainage is necessary.
The evidence for immediate incision and drainage/needle aspiration for auricular hematoma.
When consultation and referral to otolaryngology is necessary.
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Etiology and Pathophysiology
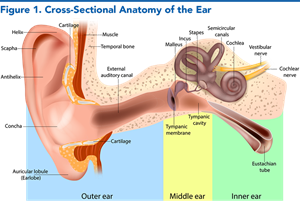
- Anatomy of the Ear
- Common Ear Pathologies
- Acute Otitis Media
- Otitis Media with Effusion
- Acute Mastoiditis
- Acute Otitis Externa
- Necrotizing Otitis Externa
- Auricular Perichondritis
- Auricular Trauma and Auricular Hematoma
- Differential Diagnosis
- Prehospital Care
- Emergency Department Evaluation
- History
- Physical Examination
- Outer Ear Examination
- Otoscopic Examination
- Equipment
- Patient Positioning
- Otoscopic Assessment
- Pneumatic Otoscopy
- Diagnostic Studies
- Laboratory Studies
- Imaging Studies
- Imaging for Acute Mastoiditis
- Imaging for Necrotizing Otitis Externa
- Treatment and Disposition
- Treatment and Disposition for Acute Otitis Media
- Managing Adult Acute Otitis Media
- Antibiotic Choice and Duration
- Pain Management
- Treatment and Disposition for Otitis Media With Effusion
- Treatment and Disposition for Acute Mastoiditis
- Treatment and Disposition for Acute Otitis Externa
- Avoidance of Ototoxic Agents
- Aural Toilet and Wick Placement
- Systemic Therapy
- Treatment and Disposition for Necrotizing Otitis Externa
- Treatment and Disposition for Auricular Perichondritis
- Treatment and Disposition for Auricular Trauma
- Treatment and Disposition for Auricular Hematoma
- Controversies and Cutting Edge
- 5 Things That Will Change Your Practice
- Risk Management Pitfalls for Emergency Department Patients With Otalgia
- Summary
- Acute Otitis Media
- Acute Mastoiditis
- Acute Otitis Externa
- Necrotizing Otitis Externa
- Auricular Hematoma
- Time- and Cost-Effective Strategies
- Case Conclusions
- Clinical Pathway for Suspected Acute Otitis Media in Pediatric Patients
- Tables and Figures
- References
Abstract
Though the vast majority of conditions associated with otalgia are not life-threatening, there are nuances and controversies in the diagnosis and management of even the most common diseases, such as acute otitis media and otitis externa. For more severe disease processes, such as necrotizing otitis externa, acute mastoiditis, and perichondritis, early recognition and timely management are paramount in reducing morbidity and mortality. A systematic approach to the evaluation of these patients is key to establishing an accurate diagnosis, identifying patients who are at high risk for dangerous etiologies or complications, and providing optimal patient care. This issue summarizes the most recent guidelines and presents a systematic, evidence-based approach to the emergency department evaluation and management of patients with otalgia.
Case Presentations
- The patient’s mother reports that the girl had a fever of 38.5°C at home earlier today, but she has remained active and is eating well. She is otherwise healthy and has never been diagnosed with otitis media before.
- Her vital signs are: temperature, 38.4C°; heart rate, 100 beats/min; blood pressure, 90/60 mm Hg; and respiratory rate, 24 breaths/min.
- Otoscopic examination shows bulging of the right tympanic membrane, with decreased mobility on insufflation. You wonder whether this patient requires antibiotics or if observation is appropriate…
- The patient reports his symptoms are not improving despite ciprofloxacin/dexamethasone otic drops. He is reporting severe otalgia, left-sided headache, as well as facial pain adjacent to his temporomandibular joint.
- He is febrile to 38.3°C upon arrival to the ED, but his other vital signs are normal.
- On examination, the external auditory canal appears macerated and edematous and there is granulation tissue visible at the osseocartilaginous junction.
- You consider whether this patient could have necrotizing otitis externa and start to plan what the next steps should be…
- The patient’s coach reports that there was no loss of consciousness during the event.
- His vital signs are: temperature, 36.8C°; heart rate, 70 beats/min; blood pressure, 118/62 mm Hg; and respiratory rate, 12 breaths/min. The neurologic examination is normal.
- On a secondary survey, you note you note a tender and fluctuant area of swelling on the anterior surface of the right pinna, with overlying ecchymosis.
- You recall that this type of traumatic injury could lead to a poor cosmetic outcome, so you start to consider what the current best-practice management strategy would be for this patient…
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
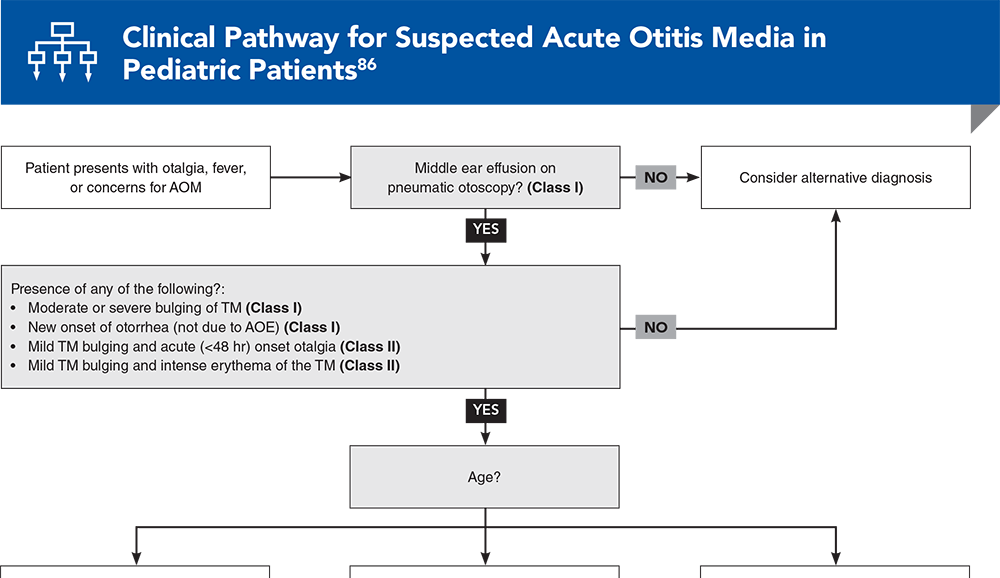
Clinical Pathway for Suspected Acute Otitis Media in Pediatric Patients
Subscribe to access the complete flowchart to guide your clinical decision making.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
10. * Rosenfeld RM, Schwartz SR, Cannon CR, et al. Clinical practice guideline: acute otitis externa. Otolaryngol Head Neck Surg. 2014;150(1 Suppl):S1-S24. (Clinical practice guideline) DOI: 10.1177/0194599813517083
14. * Long DA, Koyfman A, Long B. An emergency medicine-focused review of malignant otitis externa. Am J Emerg Med. 2020;38(8):1671-1678. (Review) DOI: 10.1016/j.ajem.2020.04.083
27. * Lieberthal AS, Carroll AE, Chonmaitree T, et al. The diagnosis and management of acute otitis media. Pediatrics. 2013;131(3):E964-E999. (Clinical practice guideline) DOI: 10.1542/peds.2012-3488
58. * Kaushik V, Malik T, Saeed SR. Interventions for acute otitis externa. Cochrane Database Syst Rev. 2010(1):CD004740. (Cochrane review; 19 randomized controlled trials, 3382 participants) DOI: 10.1002/14651858.CD004740.pub2
81. * Venekamp RP, Sanders SL, Glasziou PP, et al. Antibiotics for acute otitis media in children. Cochrane Database Syst Rev. 2015;2015(6):CD000219. (Cochrane review; 13 randomized controlled trials, 3938 AOM episodes) DOI: 10.1002/14651858.CD000219.pub4
Subscribe to get the full list of 86 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: acute, otitis, media, effusion, externa, necrotizing, mastoiditis, perichondritis, malignant, otorrhea, tympanic, diabetes