Table of Contents
About This Issue
Hematuria is a common finding in the pediatric population. There is a wide differential to consider in the emergency department. Emergency clinicians must be able to identify serious, progressive conditions while limiting unnecessary workup. This issue reviews key considerations in the evaluation and initial management of pediatric hematuria in the emergency department, including evidence-based recommendations for laboratory and imaging choices. In this issue, you will learn:
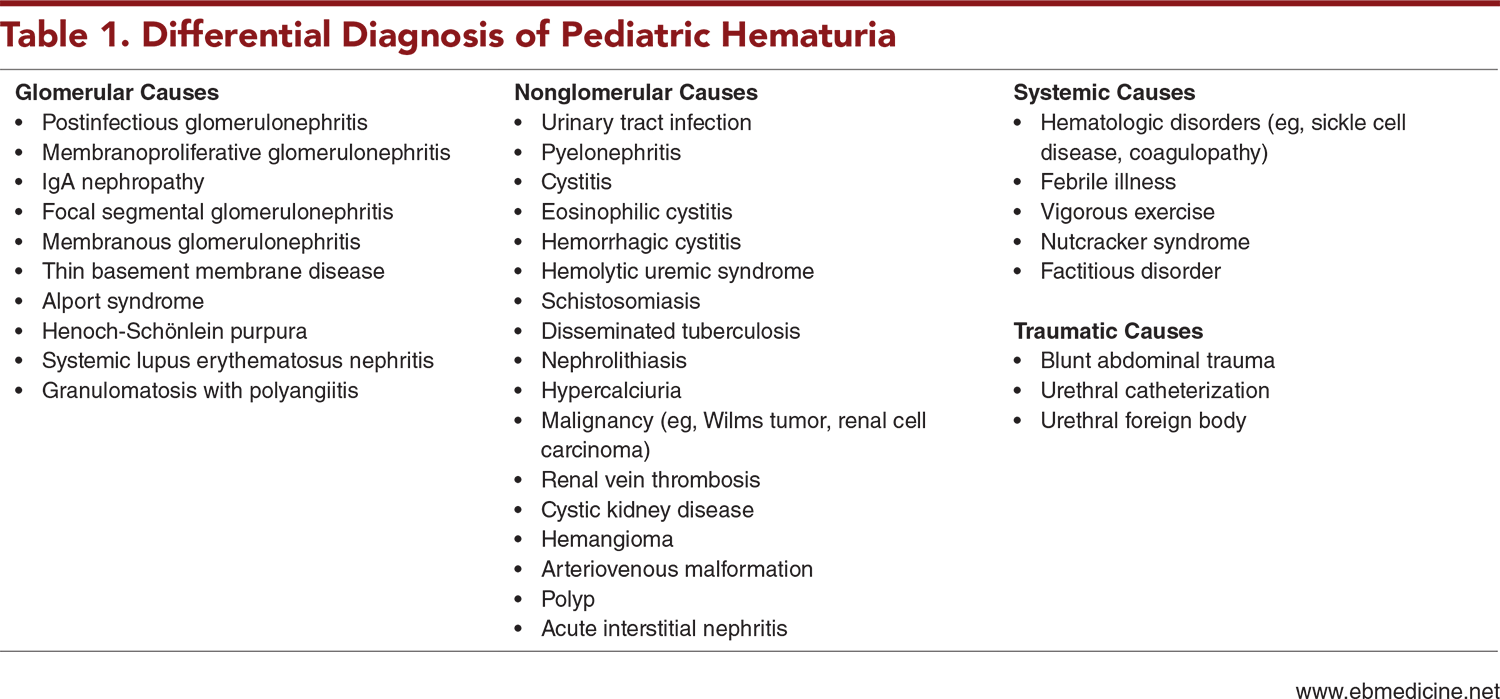
Conditions in the broad differential diagnosis of pediatric hematuria, including glomerular, nonglomerular, systemic, and traumatic etiologies
Recommendations for initial stabilization of pediatric patients with hematuria, as well as findings that are more suggestive of an underlying life-threatening condition
Important questions to ask while obtaining the history
Physical examination findings that can help narrow the differential diagnosis
General recommendations for laboratory studies, as well as specific recommendations for laboratory studies for patients with macroscopic hematuria and those with microscopic hematuria
Guidance for imaging studies, based on whether the patient has atraumatic hematuria or traumatic hematuria
Indications for referral to nephrology or urology
Special considerations for neonates and patients with underlying conditions
Which children with hematuria can be discharged safely from the ED, and which patients need to be admitted
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Etiology and Pathophysiology
- Macroscopic Hematuria
- Microscopic Hematuria
- Differential Diagnosis
- Discolored Urine Without Hematuria
- Glomerular Causes of Hematuria
- Postinfectious and Infection-Related
- Type IV Collagen Mutation
- Systemic Diseases With Renal Manifestations
- Nonglomerular Causes of Hematuria
- Infection
- Nephrolithiasis/Hypercalciuria
- Masses and Lesions
- Medications
- Systemic Causes of Hematuria
- Traumatic Causes of Hematuria
- Prehospital Care
- Emergency Department Evaluation
- Initial Stabilization
- History
- Physical Examination
- Diagnostic Studies
- Laboratory Studies
- Laboratory Studies for Macroscopic Hematuria
- Laboratory Studies for Microscopic Hematuria
- General Recommendations
- Imaging Studies
- Imaging Studies for Atraumatic Hematuria
- Imaging Studies for Traumatic Hematuria
- Additional Studies
- Treatment
- Special Populations
- Patients With Underlying Conditions
- Neonates
- Controversies and Cutting Edge
- Disposition
- 5 Things That Will Change Your Practice
- Risk Management Pitfalls for Managing Pediatric Patients With Hematuria in the Emergency Department
- Summary
- Time- and Cost-Effective Strategies
- Case Conclusions
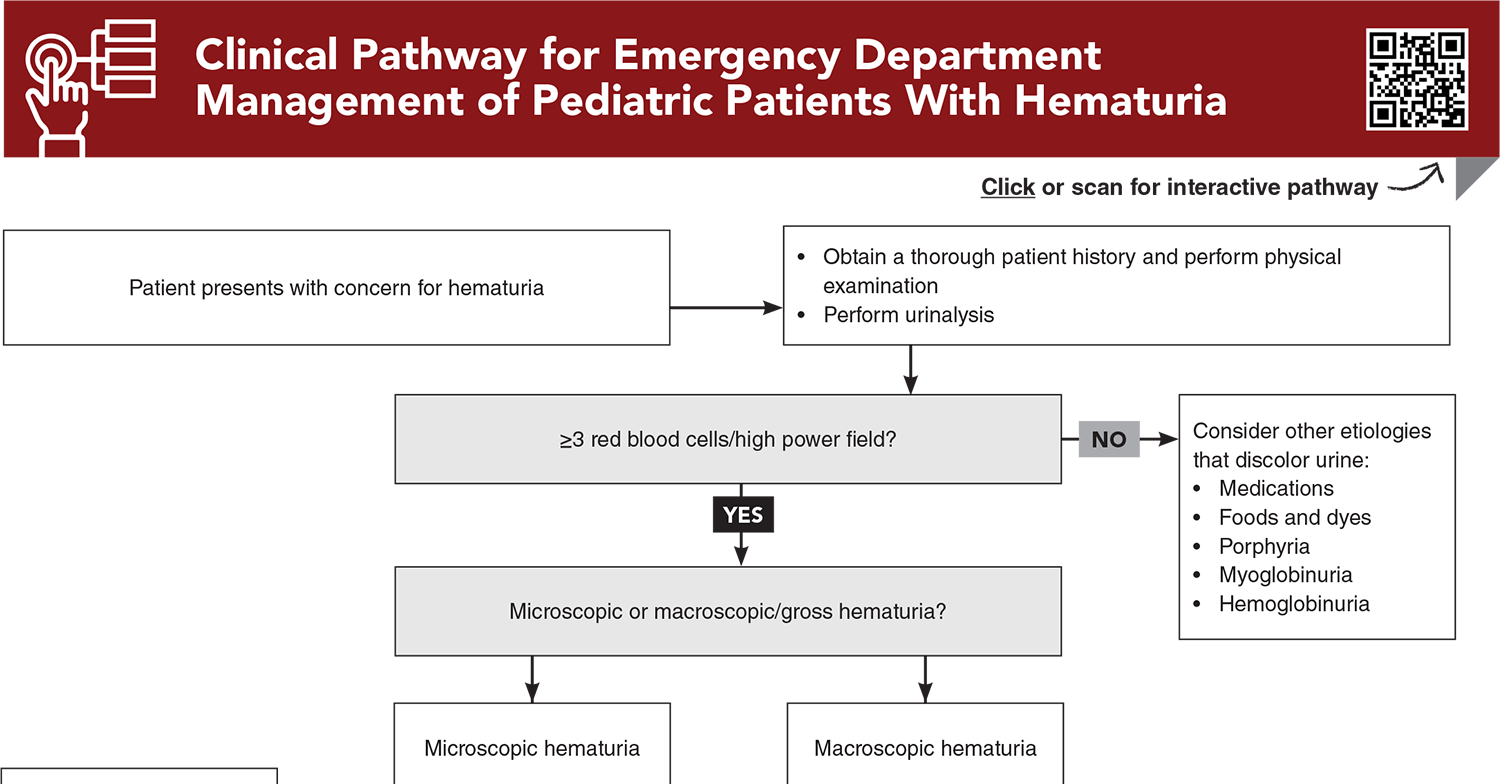
- Clinical Pathway for Emergency Department Management of Pediatric Patients With Hematuria
- Tables and Figures
- References
Abstract
Hematuria is a common finding in the pediatric population. The differential diagnosis for pediatric hematuria is wide, ranging from isolated benign causes to serious progressive renal or urologic diseases. Emergency clinicians must be able to identify high-risk features that raise suspicion for a serious underlying pathology while limiting unnecessary workup. This issue reviews key considerations in the evaluation and initial management of pediatric hematuria in the emergency department, including evidence-based recommendations on initial laboratory and imaging choices.
Case Presentations
- The boy reports a sore throat 2 weeks prior to presentation.
- His vital signs are unremarkable, except for a blood pressure of 130/68 mm Hg. On examination, you note periorbital edema. Urinalysis is positive for protein and blood.
- What workup is warranted at this time to confirm the diagnosis? What is the patient’s likely disposition?
- A review of systems is otherwise normal. The girl’s vital signs are within normal limits, and her physical examination is unremarkable, including a genitourinary examination. Urinalysis is negative for blood.
- What other questions would be helpful to confirm the diagnosis?
- The girl states she was at a rave last night but denies substance use.
- The girl’s vital signs are unremarkable. The physical examination is significant for diffuse muscle tenderness. Her urine is positive for 2+ blood.
- What other laboratory studies should be performed for this patient?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Managing Patients Presenting with Acute Diarrhea in Urgent Care
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Buy this issue and
CME test to get 4 CME credits.
Tables and Figures
Subscribe for full access to all Tables and Figures.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
2. * Imam AA, Saadeh SA. Evaluation of proteinuria and hematuria in ambulatory setting. Pediatr Clin North Am. 2022;69(6):1037-1049. (Review) DOI: 10.1016/j.pcl.2022.07.002
3. * Kallash M, Rheault MN. Approach to persistent microscopic hematuria in children. Kidney360. 2020;1(9):1014-1020. (Review) DOI: 10.34067/KID.0003222020
5. * Vedula R, Iyengar AA. Approach to diagnosis and management of hematuria. Indian J Pediatr. 2020;87(8):618-624. (Review) DOI: 10.1007/s12098-020-03184-4
6. * Brown DD, Reidy KJ. Approach to the child with hematuria. Pediatr Clin North Am. 2019;66(1):15-30. (Review) DOI: 10.1016/j.pcl.2018.08.003
8. * Mehta A, Williams V, Parajuli B. Child with dysuria and/or hematuria. Indian J Pediatr. 2017;84(10):792-798. (Review) DOI: 10.1007/s12098-017-2448-4
28. * Expert Panel on Pediatric Imaging, Dillman JR, Rigsby CK, et al. ACR Appropriateness Criteria® Hematuria-Child. J Am Coll Radiol. 2018;15(5S):S91-S103. (Guideline) DOI: 10.1016/j.jacr.2018.03.022
Subscribe to get the full list of 45 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: pediatric hematuria, gross hematuria, macroscopic hematuria, microscopic hematuria, proteinuria, glomerular hematuria, nonglomerular hematuria, systemic hematuria, traumatic hematuria, atraumatic hematuria, kidney injury, hyperkalemia, red urine, pink urine, cola-colored urine, renal disease