Table of Contents
About This Issue
Urgent care presentation of headache is common, and clinicians need to be prepared to evaluate and manage primary headaches, as well as assess for more concerning presentations such as refractory migraine, secondary causes, or headache disorders. Appropriate management of headache can streamline care, improve patient outcomes, and prevent unnecessary referrals to the emergency department. In this issue, you will learn:
The most common types of primary headache disorders, which include tension-type headache, migraine, and cluster headache, as well as medication overuse headache, a secondary headache disorder;
The difference between episodic headache and chronic headache;
The importance of a focused history, physical examination (especially a neurological examination), and clinical decision rules related to imaging studies and disposition; and
Treatment goals and pharmaceutical options for various types of primary headache disorders, including nerve blocks.
CODING & CHARTING: Factors such as severity of the headache, vital signs and associated symptoms, and underlying medical conditions influence the level of documentation required. Learn more in our monthly coding column.
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Etiology and Pathophysiology
- Tension-Type Headache
- Migraine
- Cluster Headache
- Medication Overuse Headache
- Differential Diagnosis
- Episodic Headaches
- Chronic Headaches
- Urgent Care Evaluation
- History
- Physical Examination
- Clinical Decision Rules
- Diagnostic Studies
- Laboratory Studies
- Red Flags for Urgent Transfer
- Imaging Studies
- Treatment
- Intravenous Antidopaminergic Antiemetics
- Ketorolac
- Dexamethasone
- Dihydroergotamine
- Triptans
- Novel Oral Migraine Medications
- 5-HT1F Receptor Agonist
- Anticalcitonin Gene-Related Peptide Medications
- Opioids
- Nerve Blocks
- Greater Occipital Nerve Block
- Sphenopalatine Ganglion Block
- Butalbital, Acetaminophen, and Caffeine
- Special Populations
- Older Patients
- Pregnant Patients
- Patients With Cluster Headaches
- Nerve Blocks for Cluster Headache
- Other Treatments for Cluster Headaches
- Patients With Medication Overuse Headache
- Controversies and Cutting Edge
- Development of Novel Drug Treatments
- Diagnosis of Headache Disorder
- Disposition
- Risk Management Pitfalls for Managing Primary Headaches in the Urgent Care Setting
- Summary
- Time- And Cost-Effective Strategies
- Case Conclusions
- KidBits: Urgent Care Management of Primary Headache in Children
- Urgent Care Evaluation
- Treatment
- Special Considerations
- Disposition
- References
- Critical Appraisal of the Literature
- Coding & Charting: What You Need to Know
- Determining the Level of Service
- Problems Addressed
- Complexity of Data
- Risk of Patient Management
- Documentation Tips
- Coding Challenge: Managing Primary Headache in Urgent Care
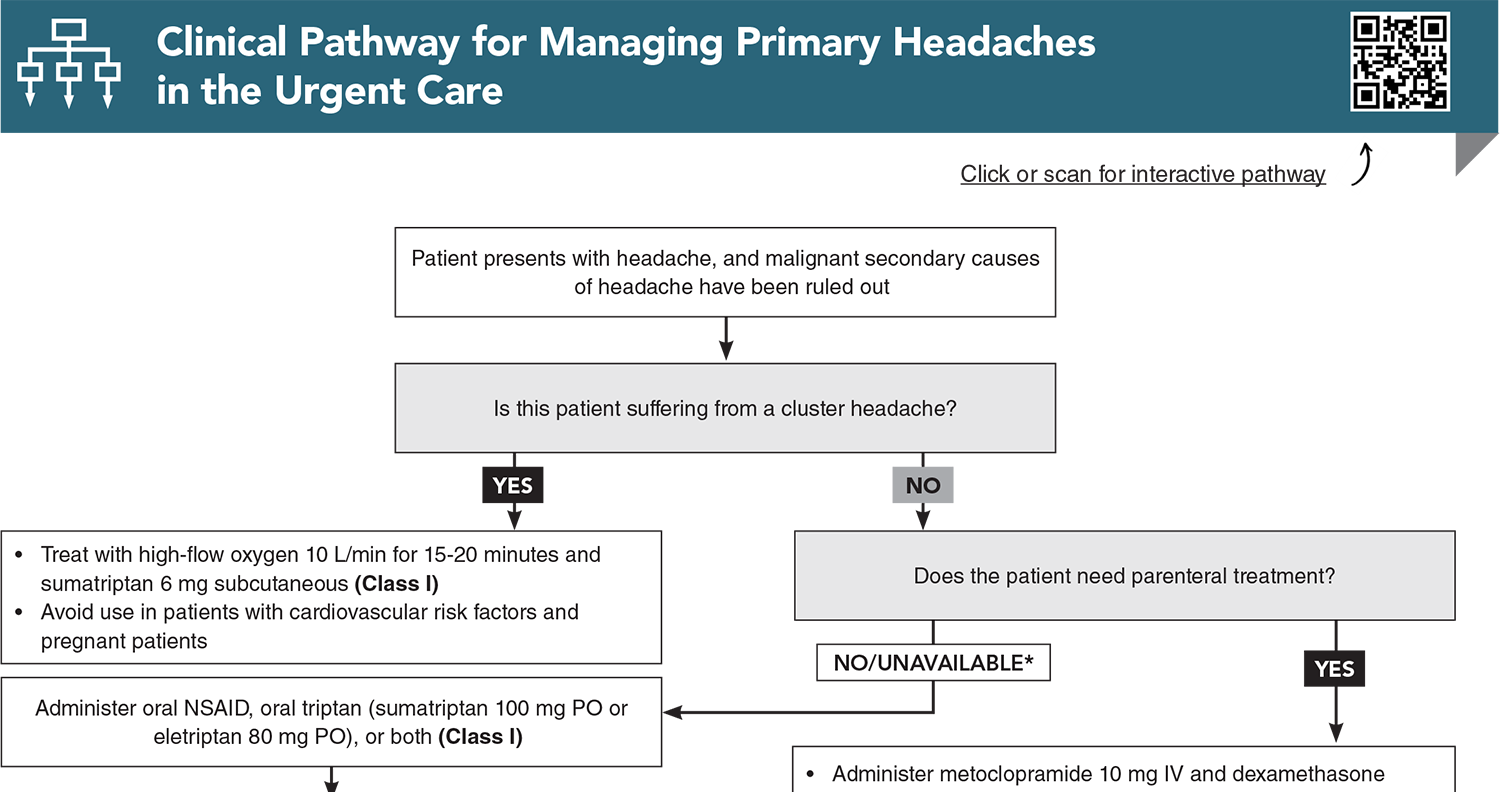
- Clinical Pathway for Managing Primary Headaches in the Urgent Care
- References
Abstract
Headache is a common presentation in urgent care. Urgent care clinicians must be prepared to evaluate and manage primary headaches, as well as rapidly assess for potentially life-threatening secondary causes that require prompt referral or transfer. This review outlines the pathology, diagnostic approach, and treatment options for migraines and other primary headaches, using the best available evidence. It covers novel medications, nerve blocks, and strategies to prevent postdrome recurrence. Headache disorders are discussed, including cluster headaches, medication overuse headaches, and chronic migraines, along with treatment options for these disorders in the urgent care setting.
Case Presentations
- She reports having similar headaches about twice monthly, and though they usually resolve with sumatriptan, she typically visits the urgent care about once a year for refractory events.
- This headache began gradually 12 hours prior and, despite taking oral sumatriptan 100 mg, ibuprofen 800 mg, and acetaminophen 1000 mg, it has not improved.
- Her physical examination is unremarkable, including normal vital signs, a normal fundoscopic and visual field examination, and a normal neurologic examination. A point-of-care urine pregnancy test is negative.
- You administer metoclopramide 10 mg IV and ketorolac 15 mg IV, but she reports only minimal relief.
- You wonder what your best next treatment option is…
- He reports an average of 3 severe headaches per year since high school, and they usually resolve completely with 10 mg oral rizatriptan.
- For the past 5 months, in association with increased stress at work, he reports an increase in headache frequency. At first, they occurred about once per week and responded to ibuprofen, but over the last month, he has had headaches nearly every day.
- Initially, he was getting relief with a combination of 10 mg oral rizatriptan once daily and 800 mg ibuprofen twice daily, but now these medications are not working at all. His headaches are associated with photophobia and phonophobia, and they are preventing him from functioning at work.
- His medical history is unremarkable, and the review of systems is otherwise normal. His physical examination, including vital signs, ophthalmologic, and neurologic examinations are normal.
- You wonder what you can offer him in the urgent care that might help…
- He has never had a headache before.
- He notes that the headache started yesterday and says he hasn’t tried anything at home for his pain yet. He says anytime he presses on his head, the pain gets worse.
- His examination is notable for a band-like distribution of the headache. He has no photophobia or phonophobia. He denies any fevers, vision changes, or vomiting.
- You administer 1000 mg PO acetaminophen, and 30 minutes later he reports marked improvement in his symptoms.
- You wonder if he requires any additional workup while he is in your urgent care…
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.
Clinical Pathway for Managing Patients Presenting with Acute Diarrhea in Urgent Care
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
9. * Loder E. Triptan therapy in migraine. N Engl J Med. 2010;363(1):63-70. (Review) DOI: 10.1056/NEJMct0910887
18. * Edlow JA, Panagos PD, Godwin SA, et al. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with acute headache. Ann Emerg Med. 2008;52(4):407-436. (Research support, non-United States government) DOI: 10.1016/j.annemergmed.2008.07.001
28. * Orr SL, Friedman BW, Christie S, et al. Management of adults with acute migraine in the emergency department: the American Headache Society evidence assessment of parenteral pharmacotherapies. Headache. 2016;56(6):911-940. (Review) DOI: 10.1111/head.12835
49. * Patel D, Yadav K, Taljaard M, et al. Effectiveness of peripheral nerve blocks for the treatment of primary headache disorders: a systematic review and meta-analysis. Ann Emerg Med. 2022;79(3):251-261. (Meta-analysis; 9 studies) DOI: 10.1016/j.annemergmed.2021.08.007
52. * Robbins MS, Starling AJ, Pringsheim TM, et al. Treatment of cluster headache: the American Headache Society evidence-based guidelines. Headache. 2016;56(7):1093-1106. (Review) DOI: 10.1111/head.12866
53. * Obermann M, Nagel S, Ose C, et al. Safety and efficacy of prednisone versus placebo in short-term prevention of episodic cluster headache: a multicentre, double-blind, randomised controlled trial. Lancet Neurol. 2021;20(1):29-37. (Randomized controlled trial; 118 patients) DOI: 10.1016/S1474-4422(20)30363-X
Subscribe to get the full list of 64 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: headache, headache disorders, episodic headache, cluster headache, tension-type headache, migraine, chronic migraine, migraine with aura, migraine without aura, primary headache, secondary headache, postdrome headache, thunderclap headache, medication overuse headache, nerve block, greater occipital nerve block, sphenopalatine ganglion nerve block, International Classification of Headache Disorders, photophobia, nausea, SNNOOP10 Criteria