Table of Contents
About This Issue
Pediatric sexual abuse is very common and may result in significant long-term physical and mental health consequences. Emergency clinicians must be able to identify pediatric sexual abuse and provide multidisciplinary medical care for these children and adolescents, including appropriate medical evaluation as well as forensic evaluation, when indicated. This issue reviews the definitions and differential diagnosis of pediatric sexual abuse, offers guidance for assessment techniques and diagnostic considerations, and provides evidence-based recommendations for management strategies for children who have experienced sexual abuse. In this issue, you will learn:
Conditions in the broad differential diagnosis of pediatric sexual abuse, including medical conditions, anatomic variations, and injuries caused by accidental trauma
Priorities of prehospital care following acute sexual abuse
Recommendations for incorporating a trauma-informed care into emergency department management of pediatric sexual abuse patients
Historical information to obtain and questions to ask the parent/guardian and patient
Guidance for examination of pediatric sexual abuse patients, including various positions and techniques that can be used to perform a pediatric anogenital examination
Recommendations for documentation and reporting
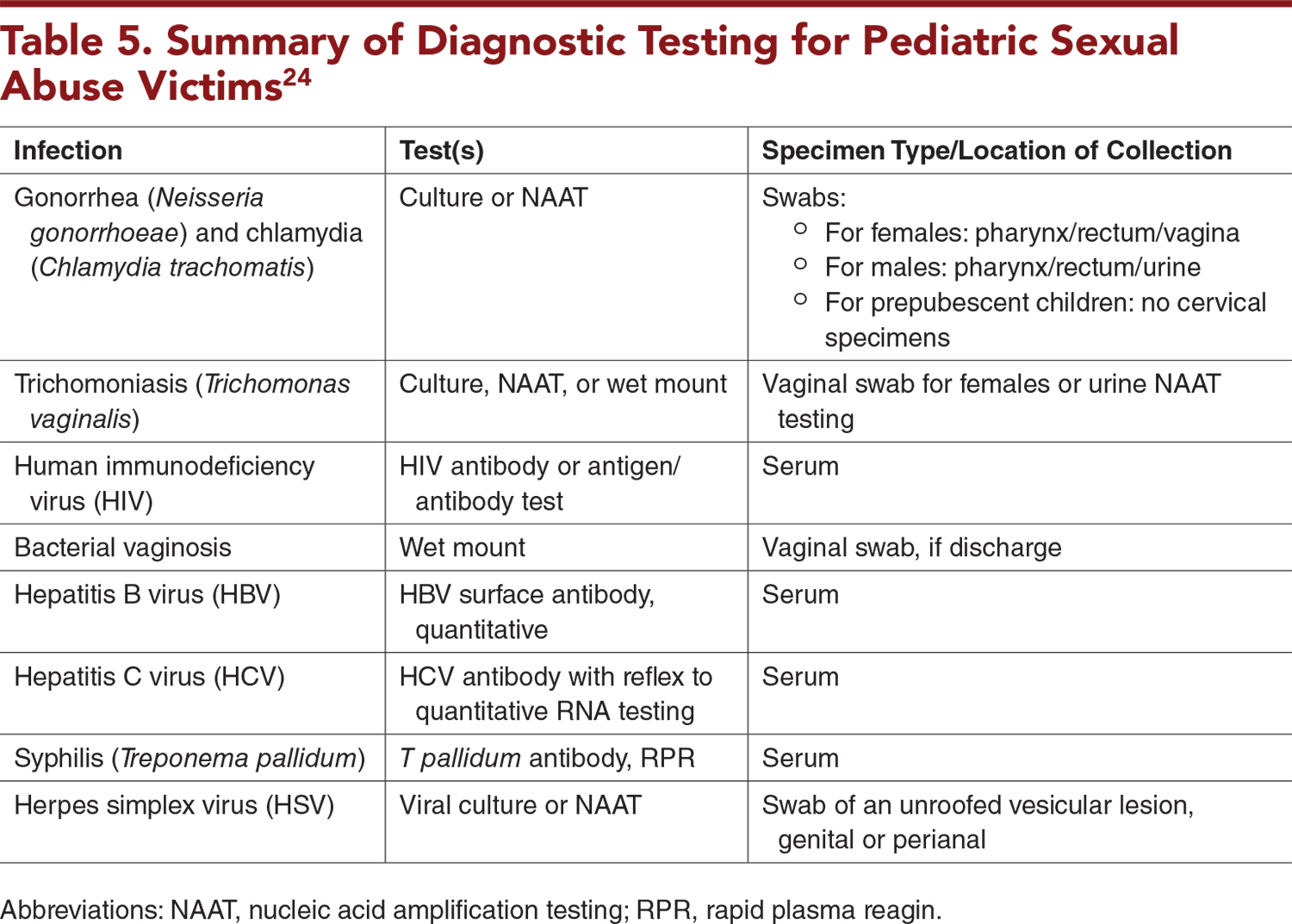
Recommendations for diagnostic testing for pediatric sexual abuse victims, including which tests should be ordered and which locations specimens should be obtained from
Which patients should receive prophylactic treatment, and which should receive treatment only after testing positive
Special considerations for victims of intimate partner violence, pregnant patients, drug-facilitation sexual assault victims, and children who are victims of human trafficking and commercial sexual exploitation
Recommendations for optimal timing for forensic evidence collection
- About This Issue
- Abstract
- Case Presentations
- Introduction
- Critical Appraisal of the Literature
- Etiology and Pathophysiology
- Differential Diagnosis
- Prehospital Care
- Emergency Department Evaluation
- Initial Evaluation and Stabilization
- Trauma-Informed Care
- History and Physical Examination
- History
- Physical Examination
- Documentation
- Diagnostic Studies
- Diagnostic Studies for Prepubescent Children
- Diagnostic Studies for Adolescent Patients
- Treatment
- Treatment for Prepubescent Patients
- Treatment for Adolescent Patients
- Pregnancy Prevention
- Vaccination
- Prophylactic Medications
- HIV Postexposure Prophylaxis for Patients of All Ages
- Treatment Side Effects and Considerations
- Special Circumstances
- Intimate Partner Violence
- Pregnant Patients
- Drug-Facilitated Sexual Assault
- Human Trafficking and Commercial Sexual Exploitation of Children
- Controversies and Cutting Edge
- Nucleic Acid Amplification Test
- Optimal Timing for Forensic Evidence Collection
- Alternate Light Sources
- Disposition
- Summary
- Risk Management Pitfalls in Emergency Department Management of Pediatric Sexual Abuse
- 5 Things That Will Change Your Practice
- Time- and Cost-Effective Strategies
- Case Conclusions
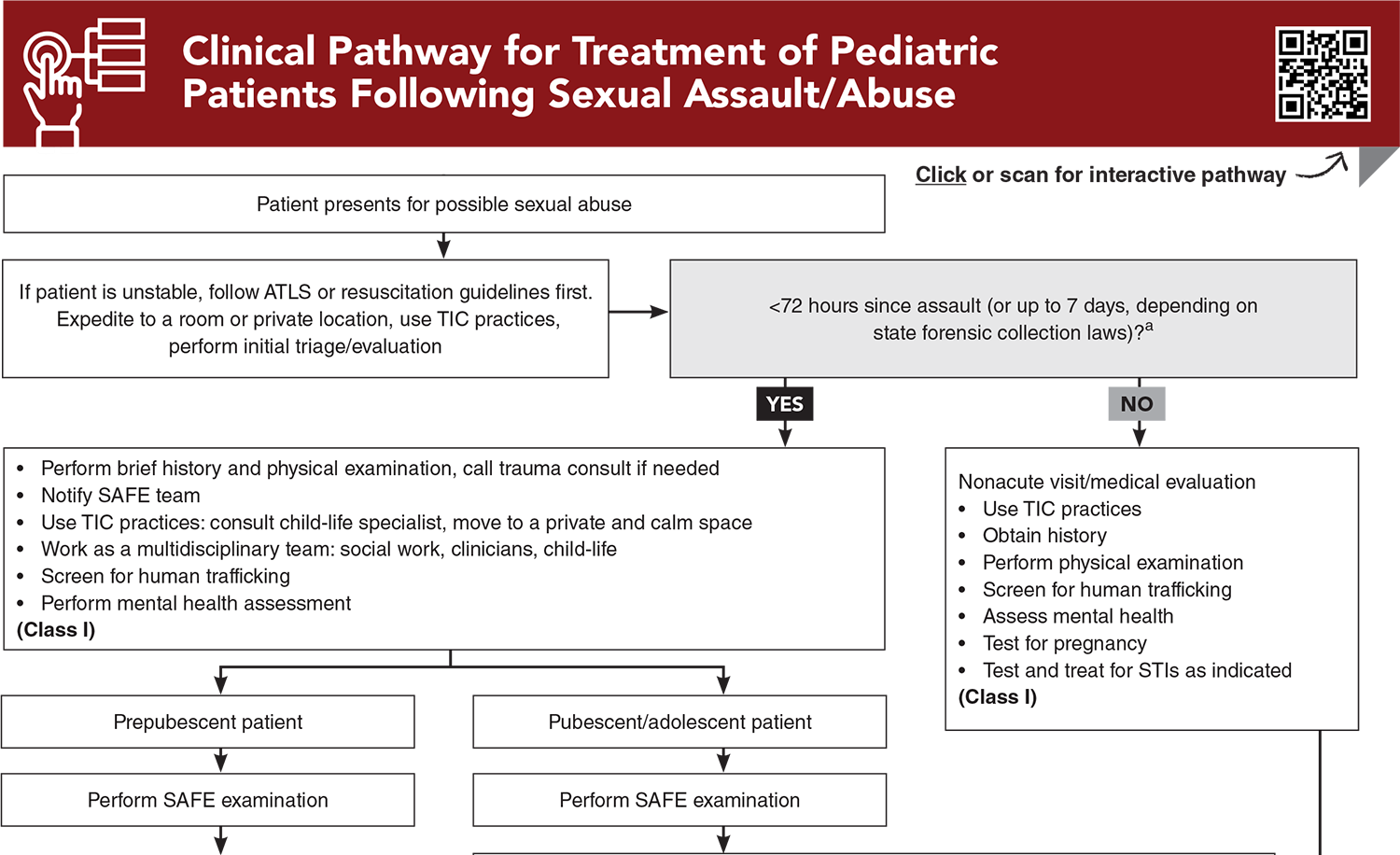
- Clinical Pathway for Treatment of Pediatric Patients Following Sexual Assault/Abuse
- Tables, Figures, and Appendix
- References
Abstract
Pediatric sexual abuse is a widespread problem impacting children and adolescents across all ages, races, ethnicities, and socioeconomic groups, and it is a topic that emergency clinicians caring for children need to be familiar with. A structured, multidisciplinary approach to the assessment, diagnosis, treatment, and follow-up of these patients is essential. This issue provides a comprehensive review of the current definitions, assessment techniques, diagnostic considerations, and management strategies for children who have experienced sexual abuse.
Case Presentations
- The child told his grandmother today that the boyfriend has been touching him in the genital area and has been asking him to engage in oral sex. The grandmother states she is concerned about the child because he has been having difficulty at school and has been more withdrawn the past 6 months after his mother’s boyfriend moved in with the family. The boyfriend is often alone with the child several evenings a week when his mother is working, most recently yesterday.
- The boy’s vital signs are unremarkable, and the child is engaged and interactive. The physical examination, including genital and rectal examination, is normal.
- What is the next step in management? What testing or treatment is indicated in this case? Whom do you need to notify?
- The patient was at a party and was given a drink by a male classmate. She remembers having a few sips of the drink and thinks that she blacked out after that. The next thing that she remembers is being in a bedroom with her clothing removed and her classmate sexually assaulting her. This happened 12 hours before arrival. She reports vaginal pain and bruises to her arms. She called her mother and told her she was raped, and her mother immediately brought her to the ED. The girl is concerned she does not remember exactly what happened and reports she drank only a half a cup of soda that a peer handed to her. The patient is requesting a rape kit and wants to press charges.
- The girl is tearful on examination, but she is alert and oriented. The girl’s vital signs are unremarkable.
- What are the next steps in ED evaluation? What special factors should you consider with this assault? What medications or treatments should you offer this patient?
- The child lives with her father, mother, and 5-year-old sister, and attends daycare 3 days a week. The mother is concerned because she noticed some redness “down there” and noticed that the child has been scratching her genital area more often this week.
- What are your next steps in evaluating this patient? What are some techniques you can utilize for physical examination of this patient? Does this patient require a SAFE examination?
How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes.

EB Medicine is excited to add a new subscriber benefit, PEMP: IRrL (In Rural Life) with real-time utility for EM clinicians, especially those practicing in rural settings. This supplemental content will focus on challenges and solutions when the pressure is on and resources are limited. Learn more about PEMP: IRrL here.
Clinical Pathway for Treatment of Pediatric Patients Following Sexual Assault/Abuse
Subscribe to access the complete Clinical Pathway to guide your clinical decision making.
Tables, Figures, and Appendix
Subscribe for full access to all Tables and Figures.
Buy this issue and
CME test to get 4 CME credits.
Key References
Following are the most informative references cited in this paper, as determined by the authors.
3. * The Administration for Children and Families. Child maltreatment 2022. Accessed April 1, 2025. (Review)
21. * Kellogg N. The evaluation of sexual abuse in children. Pediatrics. 2005;116(2):506-512. (Practice guideline) DOI: 10.1542/peds.2005-1336
23. * United States Centers for Disease Control and Prevention. STD treatment guidelines child sexual assault. 2021. Accessed April 1, 2025. (Practice guideline)
24. * United States Centers for Disease Control and Prevention. Sexual assault and abuse and STIs-adolescents and adults 2021. Accessed April 1, 2025. (Practice guideline)
26. * United States Centers for Disease Control and Prevention. Summary of CDC STI treatment guidelines. 2021. Accessed April 1, 2025. (Practice guideline)
28. * United States Centers for Disease Control and Prevention. Sexually transmitted infections treatment guidelines, 2021. 2021. Accessed April 1, 2025. (Practice guidelines)
48. * Greenbaum VJ, Dodd M, McCracken C. A short screening tool to identify victims of child sex trafficking in the health care setting. Pediatr Emerg Care. 2018;34(1):33-37. (Cross-sectional; 108 patients) DOI: 10.1097/pec.0000000000000602
53. * Kellogg ND, Melville JD, Lukefahr JL, et al. Genital and extragenital gonorrhea and chlamydia in children and adolescents evaluated for sexual abuse. Pediatr Emerg Care. 2018;34(11):761-766. (Cross-sectional; 1319 patients) DOI: 10.1097/pec.0000000000001014
Subscribe to get the full list of 67 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource.
Keywords: sexual abuse, pediatric sexual abuse, sexual assault, sexual assault forensic examiner (SAFE), sexual assault nurse examiner, SANE, sexual assault examiner, SAE, sexual assault response team, SART, adverse childhood experiences, trauma-informed care, physical examination positions, documentation, gonorrhea, chlamydia, trichomoniasis, human immunodeficiency virus, HIV, HIV postexposure prophylaxis, bacterial vaginosis, hepatitis B, hepatitis C, syphilis, herpes simplex virus, HSV, intimate partner violence, drug-facilitated sexual assault, sexual violence, sexual exploitation, human trafficking, commercial sexual exploitation of children, CSEC, child abuse, child maltreatment, rape, genital injury, nucleic acid amplification test, NAAT, alternate light sources